What Is Eczema? Signs, Drives, Assessments, Medication, and Preventative.
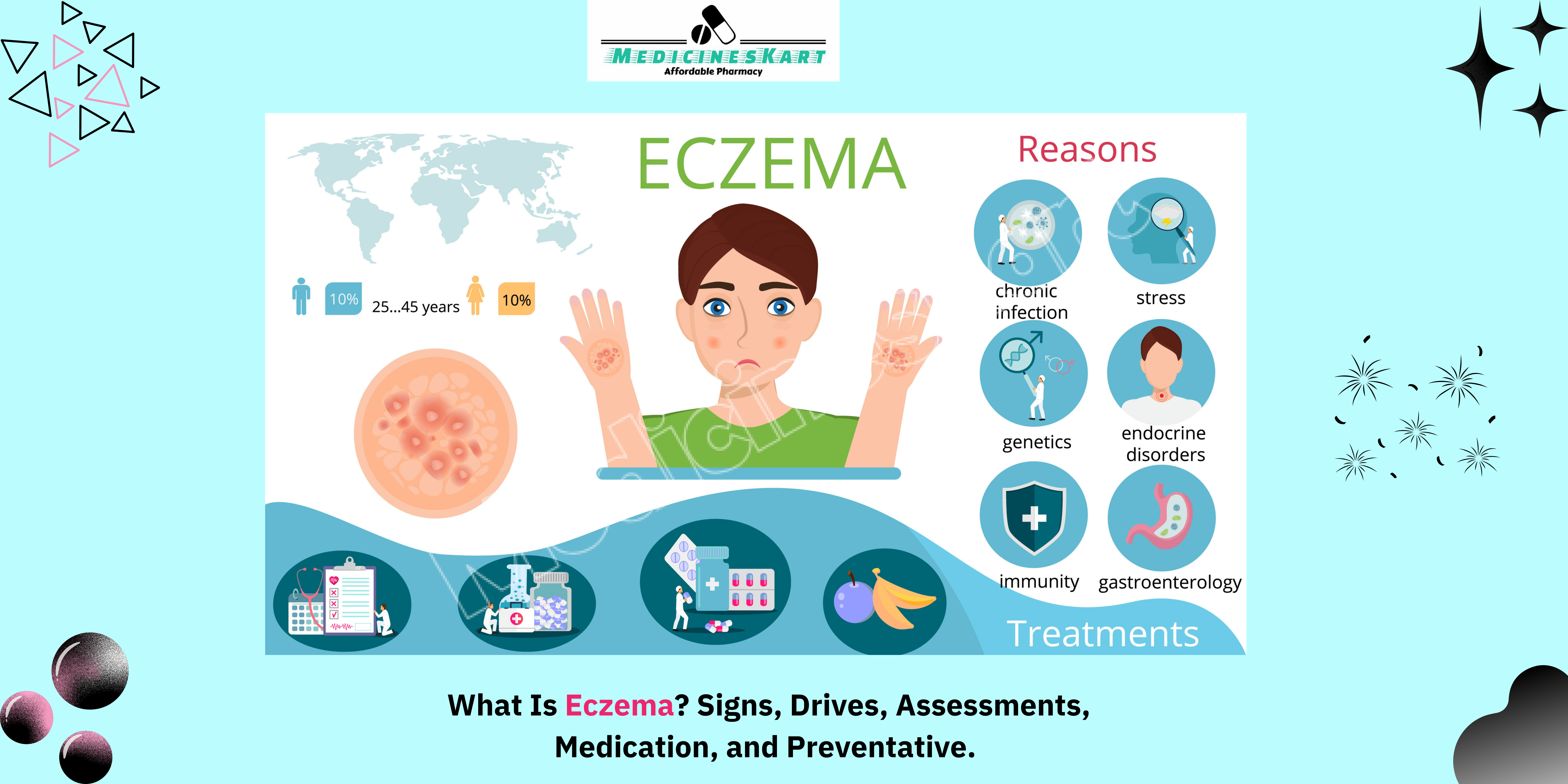
What Is Eczema?
Eczema, also known as atopic dermatitis, is a chronic skin condition characterized by inflamed, itchy, and sometimes painful patches of skin. It’s a non-contagious disorder that affects people of all ages, though it’s particularly common in children. Eczema can vary in severity, ranging from mild cases that cause occasional discomfort to severe forms that significantly impact quality of life. While there is no cure for eczema, proper management and treatment can help control flare-ups and minimize symptoms.
The condition can appear anywhere on the body but is most often found on the face, hands, feet, inner elbows, and behind the knees. Eczema is part of the “atopic triad,” which includes asthma and hay fever, meaning that people with eczema are more likely to have or develop these conditions.
Signs and Symptoms of Eczema
The symptoms of eczema can vary depending on the individual, the severity of the condition, and the specific type of eczema present. However, the most common signs include:
- Dry, Flaky Skin:
- One of the hallmark signs of eczema is dry skin, which can become flaky and rough. The skin may feel tight or sensitive, especially after bathing or exposure to cold, dry air.
- Itching:
- Itching is perhaps the most defining symptom of eczema. It can range from mild to severe and is often worse at night. Scratching the affected areas can exacerbate the condition, leading to a vicious cycle of itching and scratching.
- Red, Inflamed Skin:
- Eczema flare-ups often cause red or darkened areas of skin that are swollen or inflamed. These patches may feel warm to the touch and can be quite uncomfortable.
- Rashes:
- During a flare-up, eczema often manifests as rashes, which may appear in patches or cover large areas of the skin. These rashes can range from small bumps to larger raised areas and may even blister or ooze in more severe cases.
- Thickened or Scaly Skin:
- Over time, chronic scratching and inflammation can lead to skin thickening, also known as lichenification. The affected skin becomes leathery and more prone to cracking, which can cause additional discomfort.
- Crusting and Oozing:
- In cases of severe eczema, the skin may develop open sores that ooze clear or yellowish fluid. These areas can crust over as the skin tries to heal. If not properly managed, they may become infected, causing further complications.
- Hyperpigmentation or Hypopigmentation:
- Long-term eczema can lead to changes in skin color, either darkening or lightening the affected areas. This is more common in people with darker skin tones and can take time to resolve even after inflammation subsides.
- Location-Specific Symptoms:
- The location of eczema on the body can affect how it presents. For example, facial eczema may cause redness and irritation around the eyes and mouth, while hand eczema can result in cracked, painful skin that’s exacerbated by washing and exposure to irritants.
Drives and Triggers of Eczema
Eczema is influenced by a combination of genetic, environmental, and immune system factors. Understanding the triggers that drive flare-ups is crucial for managing the condition effectively.
- Genetics:
- Eczema tends to run in families, particularly those with a history of allergic conditions like asthma and hay fever. If a parent or sibling has eczema, there is an increased likelihood that an individual will develop it as well. Genetic mutations affecting the skin’s barrier function are thought to contribute to the condition, making the skin more vulnerable to irritants and allergens.
- Immune System Dysregulation:
- Eczema is an immune-mediated condition, meaning the immune system overreacts to certain triggers, leading to inflammation in the skin. People with eczema often have higher levels of certain immune cells, like T-cells, that cause the body to attack its own skin cells, resulting in the characteristic symptoms of the condition.
- Environmental Triggers:
- Environmental factors play a significant role in eczema flare-ups. Common triggers include:
- Weather: Cold, dry air can strip moisture from the skin, while heat and humidity can cause sweating, which may irritate the skin.
- Allergens: Exposure to dust mites, pollen, pet dander, mold, and other allergens can trigger eczema, especially in people with allergies.
- Irritants: Harsh soaps, detergents, perfumes, and cleaning products can exacerbate eczema by stripping away the skin’s natural oils, leading to dryness and irritation.
- Fabric: Certain fabrics, like wool and synthetic materials, can cause irritation and trigger flare-ups. Loose, soft, breathable clothing, such as cotton, is generally recommended for individuals with eczema.
- Environmental factors play a significant role in eczema flare-ups. Common triggers include:
- Stress:
- Emotional stress can trigger or worsen eczema symptoms. The exact mechanism isn’t fully understood, but stress is known to activate the immune system and increase inflammation, leading to more intense flare-ups.
- Food Allergies:
- In some individuals, eczema may be triggered by food allergens. This is more common in infants and children, with dairy, eggs, peanuts, soy, and wheat being common culprits. Identifying and avoiding specific food triggers can help reduce flare-ups.
- Infections:
- Skin infections, particularly bacterial (such as Staphylococcus aureus), fungal, or viral infections, can worsen eczema or lead to more severe outbreaks. This is because broken skin due to scratching provides a way for microbes to enter the body, leading to infections that cause further inflammation.
- Hormonal Changes:
- Fluctuations in hormones, particularly in women, can impact eczema. Some women notice an increase in symptoms during pregnancy, menstruation, or menopause due to changes in hormone levels.
Assessments and Diagnosis
Diagnosing eczema is largely based on the presentation of symptoms and a thorough medical history. There is no specific test for eczema, but a healthcare provider can usually diagnose the condition through a combination of visual examination and patient interviews.
- Physical Examination:
- A dermatologist or general physician will examine the skin to assess the type and severity of the rash. They may ask about when the symptoms started, what triggers seem to worsen the condition, and any family history of eczema or other allergic conditions.
- Patch Testing:
- In some cases, a patch test may be used to determine if certain substances are causing an allergic reaction. This involves applying small amounts of suspected allergens to the skin and monitoring for any reaction. Patch testing can help identify contact allergens that might be exacerbating eczema.
- Blood Tests:
- Although not routinely used to diagnose eczema, blood tests might be ordered to check for elevated levels of immunoglobulin E (IgE), an antibody associated with allergic responses. High IgE levels can indicate an allergic component to the patient’s eczema.
- Skin Biopsy:
- In rare cases, a skin biopsy may be performed to rule out other skin conditions that mimic eczema, such as psoriasis or fungal infections. A small piece of skin is removed and examined under a microscope.
Medication and Treatments for Eczema
While there is no cure for eczema, there are a variety of treatments aimed at managing symptoms and preventing flare-ups. Treatment plans are often tailored to the individual and may include topical, oral, and systemic therapies.
- Moisturizers and Emollients:
- Keeping the skin well-hydrated is one of the most important steps in managing eczema. Moisturizers and emollients help restore the skin barrier and prevent moisture loss, reducing dryness and itching. It’s important to use thick, fragrance-free moisturizers immediately after bathing to lock in moisture.
- Topical Steroids:
- For more severe flare-ups, topical corticosteroids are commonly prescribed to reduce inflammation and relieve itching. These come in various strengths, and long-term use should be monitored to avoid side effects such as skin thinning.
- Topical Calcineurin Inhibitors:
- For sensitive areas like the face and eyelids, calcineurin inhibitors like tacrolimus and pimecrolimus can be used as an alternative to steroids. They help suppress the immune response that leads to inflammation without the long-term side effects associated with steroid use.
- Antihistamines:
- Oral antihistamines can help relieve itching, especially at night, allowing for better sleep. While they do not treat the underlying inflammation, they can make symptoms more manageable.
- Oral Steroids and Immunosuppressants:
- For severe or widespread eczema, oral corticosteroids or immunosuppressive medications like cyclosporine or methotrexate may be prescribed. These are typically used for short periods due to their potential side effects.
- Biologic Therapies:
- For individuals with severe eczema that does not respond to traditional treatments, biologics such as dupilumab (Dupixent) can be used. These drugs target specific components of the immune system to reduce inflammation and are generally reserved for people with moderate to severe cases.
- Phototherapy:
- Ultraviolet (UV) light therapy can help reduce eczema symptoms in some individuals by slowing down the immune response in the skin. This treatment is typically done in a clinical setting under medical supervision.
- Antibiotics and Antifungals:
- If eczema becomes infected, antibiotics or antifungal medications may be required to treat the infection. Keeping the skin clean and avoiding excessive scratching can help prevent infection.
Preventative Measures for Eczema
Preventing eczema flare-ups involves a combination of lifestyle adjustments, skincare routines, and avoiding known triggers.
- Maintain a Regular Skincare Routine:
- Daily moisturizing is essential to keep the skin hydrated and healthy. Using gentle, fragrance-free products can help prevent irritation and dryness.
- Avoid Known Triggers:
- Identifying and avoiding environmental and dietary triggers can reduce the frequency and severity of eczema flare-ups. This may involve using hypoallergenic bedding, avoiding harsh soaps, and steering clear of certain foods.
- Manage Stress:
- Since stress can worsen eczema, finding ways to manage stress through relaxation techniques, exercise, or counseling can be beneficial.
- Wear Soft, Breathable Fabrics:
- Wearing loose-fitting, breathable clothing made from natural fibers like cotton can help prevent skin irritation. Avoid wool, polyester, and other rough materials that can exacerbate symptoms.
- Stay Hydrated:
- Drinking plenty of water throughout the day can help keep the skin hydrated from the inside out, supporting overall skin health.
- Use a Humidifier:
- In dry environments, using a humidifier can help add moisture to the air, reducing the drying effect on the skin.


Leave a Reply